What is the connection between shingles and the COVID-19 vaccine? - Medical News Today
Shingles is an uncomfortable common condition that causes a characteristic rash, among other symptoms. Some studies suggest a link between COVID-19 vaccines and reactivation of the virus that causes shingles. While evidence suggests this could be possible, it is at the very least uncommon.
Shingles is a fairly common condition that may affect roughly 20–30% of people in their lifetime, with the risk of developing shingles
Several case reports note people experiencing a shingles flare-up after receiving a COVID-19 vaccine. While evidence cannot attribute the flares to the vaccine, it may be possible that the immune response to the vaccine might trigger a flare. Some studies suggest this may not be an adverse event and just a coincidence. However, more research is still necessary to investigate the association.
In this article, we will discuss the possible association between COVID-19 vaccines and the reactivation of VZV.
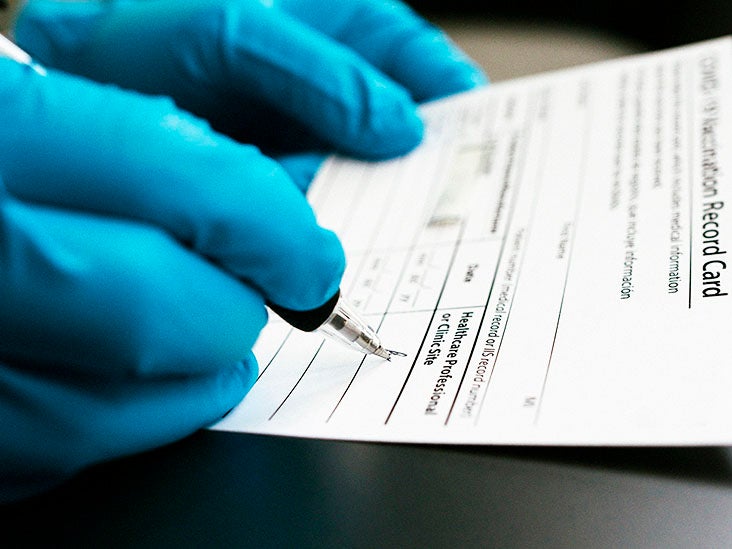
To help prevent the transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), health experts advise that people receive a COVID-19 vaccine as soon as possible. While the Centers for Disease Control and Prevention (CDC) state that the vaccines are
Researchers continue to
A
They note that following vaccination, some people may experience lymphocytopenia or lower levels of white blood cells. The researchers add that this temporary period of lymphocytopenia may be sufficient to trigger VZV reactivation and result in a shingles flare.
This is consistent with another
Furthermore, a 2021 paper on older adults and a 2021 case series on people with an autoimmune condition highlight cases of shingles following COVID-19 vaccination. While the studies cannot prove causality, they suggest that it could be a plausible but rare AEAV. While more research is necessary, these findings may indicate the requirement for further vigilance and safety monitoring, particularly for those at higher risk of shingles.
Other research also highlights the potential role that stress may play. Stressors from social restrictions, new variants, and the process of vaccination may contribute towards affecting the immune response.
However, current evidence cannot attribute a definitive link between the two, and the CDC still recommends COVID-19 vaccination for all people aged 5 and older. Even if there is an association, it is a rare side effect, and the benefits of vaccination outweigh the potential risks.
It is also worth noting that COVID-19 vaccines do not cause shingles, and a person will not directly acquire shingles from a COVID-19 vaccine. If the events are related, they will only occur in individuals with dormant VZV from a previous case of chickenpox or shingles.
Symptoms of shingles
The term
People may experience a variety of symptoms of COVID-19, such as fever and coughing, that might appear 2–14 days after exposure to SARS-CoV-2. Some individuals may also
Due to the potential health risk of COVID-19, scientists were able to develop
Shingles results from the reactivation of VZV. After recovery from chickenpox, the virus lays dormant in the sensory ganglia of the cranial nerve or the dorsal root ganglia within the peripheral nervous system. The virus can hide in the nervous system, where it can remain indefinitely in a dormant state.
Like waking up from hibernation, the virus can reactivate and travel down nerve fibers to cause a new active infection. At present, the trigger for reactivation is
Anyone who believes that they have developed shingles should contact a doctor as soon as possible. A doctor will be able to diagnose shingles and provide appropriate treatment.
In many cases, a primary care physician can manage shingles care, but people may require specialist care in some cases. Getting treatment shortly after the onset of symptoms can help decrease the duration and severity of the infection. It can also help prevent potential
There are many treatment options available for shingles. Typically, a doctor may recommend antiviral medications, as they can help treat shingles and shorten the length and severity of the illness. Antivirals that can treat shingles
Additionally, there are many home remedies people can try to help alleviate discomfort. These can include cool oatmeal baths, using calamine lotion, and trying to avoid stress.
While the link is unclear, some reports suggest a connection between COVID-19 vaccines and shingles eruptions. Although there is not enough evidence to suggest causality, some researchers indicate that the immune response to the vaccine may trigger a shingles flare. However, more research is necessary.
Shingles occurs after the reactivation of the varicella-zoster virus occurs due to an unknown trigger. Some evidence notes that changes to the immune system could be the trigger that reactivates the virus.
Despite this potential link, health experts advise that people still receive a COVID-19 vaccine as soon as possible. This is because the benefit of the vaccine outweighs the potential risks. Additionally, the vaccine cannot cause a person to acquire shingles. A person can only develop shingles if they have experienced a previous case of chickenpox or shingles.
Comments
Post a Comment