Epstein-Barr virus infection-associated cholangiocarcinoma: a report of one case and the review of literature - Virology Journal - Virology Journal
A 36-year-old female patient was admitted to the Department of Hepatobiliary Surgery, Affiliated Hangzhou First People's Hospital, Zhejiang University School of Medicine on April 28, 2021 with complaints of middle and upper abdominal pain and discomfort for more than 1 month combined with systemic skin yellowing with skin itching for 2 weeks. One month ago, the patient had middle and upper abdominal pain and discomfort without obvious inducement, which was intolerable. She visited Zhongshan Hospital, Fudan University. CA199:101.0 U/ml, AFP: 4.5 ng/ml. Abdominal CT showed multiple space-occupying lesions in the liver, PET-CT showed multiple MTs, hilar lymph node metastasis in the liver, and cervical lymphadenitis. Liver mass puncture was performed, On April 7, 2021, pathology report showed: consider poorly differentiated carcinoma, and it is recommended to consider primary poorly differentiated carcinoma of the liver after clinical exclusion of metastasis. Immunohistochemistry: Hepa (partially weak+), ARG-1 (−), CK7 (−), CK19 (+), CK20 (−), CDX2 (bits of weak +), p63 (−), p40 (−), SATB2 (weak+), Ki-37 (80% positive), Syn (−), CgA (−), CD56 (−), GATA3 (weak+), PAX8 (−), TTF-1 (−), NapsinA (−), a-Inhibin (−), S-100 (−), SF1 (+), ER (−), PR (−), CK {pan} (+), CK8 (+), SALL4 (individual weak +), CD30 (−), PAX-5 (−), SMA (−), Des (weak +), HMB-45 (−), AFP (−), LCA (lymphocyte +), OCT-4 (−), PLAP (−), CD34 (−). The patient did not receive further treatment. Two weeks ago, the patient developed gradually aggravated abdominal pain, yellow sclera and yellowish skin all over the body, with skin itching. The patient visited to our department for further treatment, and was admitted to the outpatient department for liver malignant tumor. The patient had a history of diabetes for 1 year and was regularly treated with 1 tablet of metformin (Tid) and 1 tablet of acarbose (Tid) orally. Physical examination on admission: right upper quadrant tenderness +, no rebound tenderness, no enclosed mass, negative Murphy's sign, and negative shifting dullness.
Laboratory tests after admission: liver function: alanine aminotransferase 242 U/L, aspartate aminotransferase 404 U/L, r-glutamyltransferase 1516 U/L, total protein 63.4 g/L, albumin 27.6 g/L, globulin 35.8 g/L, total bilirubin 308.2 µmol/L, conjugated bilirubin 224.9 µmol/L, indirect bilirubin 83.3 µmol/L, lactate dehydrogenase 3433 U/L, C-reactive protein 23.5 mg/L, and HbA1c glycosylated hemoglobin 6.4%. Blood coagulation routine: prothrombin time 15.1 s, international normalized ratio 1.42, D-dimer 350.0 µg/L. Blood routine: WBC: 12.7 * 109/L, NEU: 81.9%, hemoglobin: 89 g/L, RBC: 3.48 * 1012/L, PLT: 593 * 109/L. Chest CT: pulmonary nodules, exudation in both lower lobes, bilateral pleural reactions, a small amount of right pleural effusion. Contrast-enhanced CT of the abdomen: diffuse mass-like and nodular slightly hypodense lesions, some of which were fused, with significant ring enhancement in the arterial phase, continuous ring enhancement in the venous and delayed phases, and local wall thinning and irritability in the right and left branches of the portal vein. The hepatobiliary ducts were dilated, and the gallbladder wall was thickened and edematous. Malignant tumors were considered, with a high possibility of hepatocellular carcinoma or cholangiocarcinoma, with local invasion of the right and left branches of the portal vein, hilar lymphadenopathy, and a small amount of ascites (see Fig. 1). Abdominal ultrasound: multiple hypoechoic masses in liver, possibility of liver cancer, irritable gallbladder wall, hypoechoic nodules in front of the pancreas, considering enlarged lymph nodes (see Fig. 2). Contrast-enhanced MR of the liver: diffuse nodular mass shadows in the liver, and contrast-enhanced scans showed mild enhancement of nodular mass shadows and ring-like enhancement changes. Consider malignant tumor combine with intrahepatic multiple metastases, the left branch of the portal vein was not clearly displayed, consider possible involvement; the right branch of the portal vein was suspect been locally invaded, the hepatic vein and the bile duct in the hilar area were not clearly displayed, the bile duct at the upper level was slightly dilated, the left upper quadrant was turbid, with the possibility of local nodules (see Fig. 3).
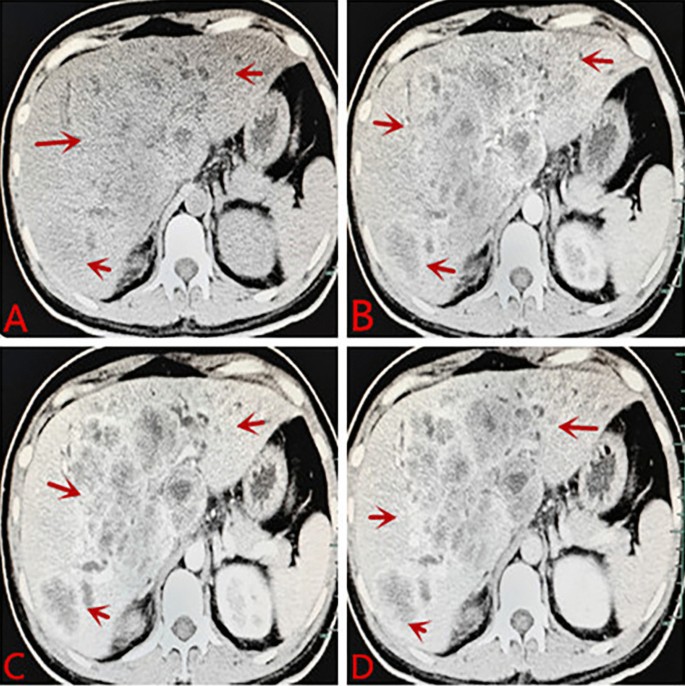
A Plane CT scan indicates less regular shape of liver, diffuse mass-like and nodular slightly hypodense lesions, some of which were fused. B Contrast-enhanced CT: significant ring enhancement in the arterial phase. C, D Continuous ring enhancement in the venous and delayed phases, local wall thinning and irritability in the right and left branches of the portal vein. Consider malignant tumors, a high possibility of hepatocellular carcinoma or cholangiocarcinoma, with local invasion of the right and left branches of the portal vein, hilar lymphadenopathy, and a small amount of ascites
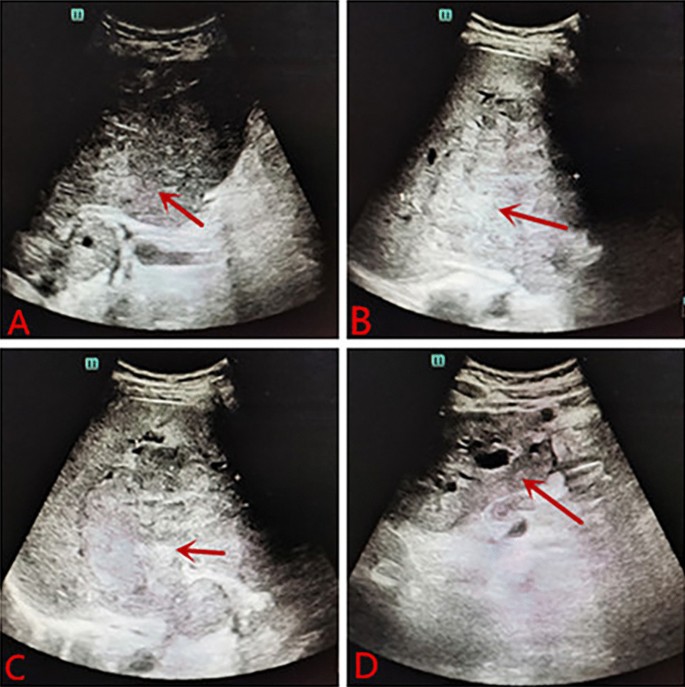
A Abdominal ultrasound: size increased liver, and multiple hypoechoic masses observed. B–D Multiple hypoechoic masses in liver, the large intrahepatic mass is about 11.5 * 10.8 * 10.2 cm, located at the right, consider the possibility of liver cancer
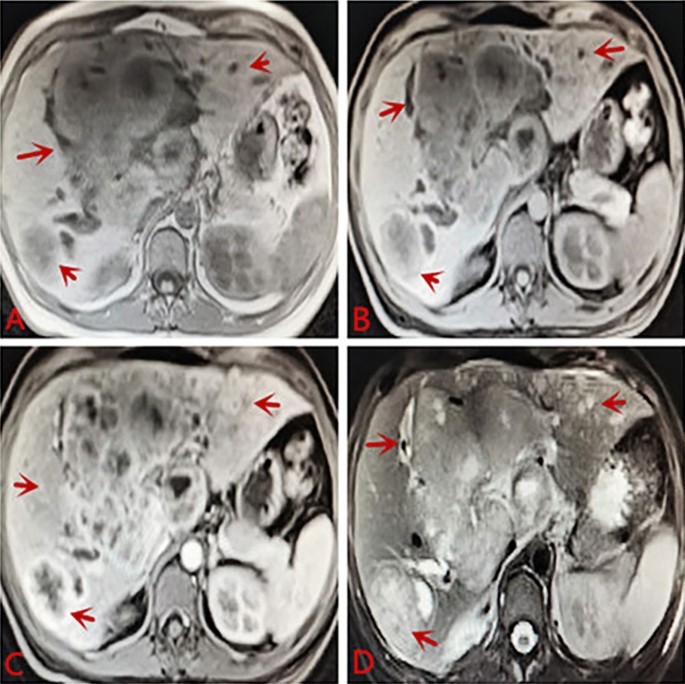
A Plain MRI scan: increased liver volume with multiple nodules and mass shadows inside, showing slightly long T1 and slightly long T2 signals, liquefaction necrosis changes were observed in the center of the lesion, and some lesions appeared to be fused. B–D Contrast-enhanced scans showed mild enhancement of nodular mass shadows and ring-like enhancement changes. Consider malignant tumor combine with intrahepatic multiple metastases. The left branch of the portal vein was not clearly displayed, consider possible involvement. The right branch of the portal vein was suspect been locally invaded, the hepatic vein and the bile duct in the hilar area were not clearly displayed, the bile duct at the upper level was slightly dilated, the left upper quadrant was turbid, consider the possibility of local nodules
The patient was given ademetionine 1000 mg Qd for choleresis treatment, vitamin K1iInjection 30 mg Qd for thromboprophylaxis, cefoperazone sodium and sulbactam sodium injection 2g Q8h for anti-infection. Transfusion of type O RH positive suspended red blood cells was given to repair anemia and coagulation abnormalities. On May 1, 2021, ultrasound-guided biliary drainage was performed for jaundice reduction treatment, and the right bile duct PTCD conditions were immature. After surgery, the PTCD drainage tube was patent, and the icteric skin and sclera gradually improved. Liver puncture pathology revealed infiltrative growth of significant heterocyst nests in the liver tissue, which was morphologically consistent with malignant tumors, and poorly differentiated carcinoma was considered. Pathology suggestion: combining liver puncture with morphology, immunohistochemistry, and EBV in situ hybridization results, it was consistent with EB virus-associated poorly differentiated carcinoma (See Fig. 4). Consider EBV infection-associated poorly differentiated cholangiocarcinoma (LELC morphology). Immunohistochemical results: CK7 foci (+), CK18 (weak + - +), CK19 (weak + - +), CK20 (−), CDX2 (weak + - +), AFP (−), Hepar1 (−), Arg-1 (−), GATA-3 (−), Vim (-), P40 a little (+), CD117 (−), CerbB2 (−), Ki-67 (+) 80%-90%, EBV in situ hybridization: tumor cells EBER (+) (Fig. 5).
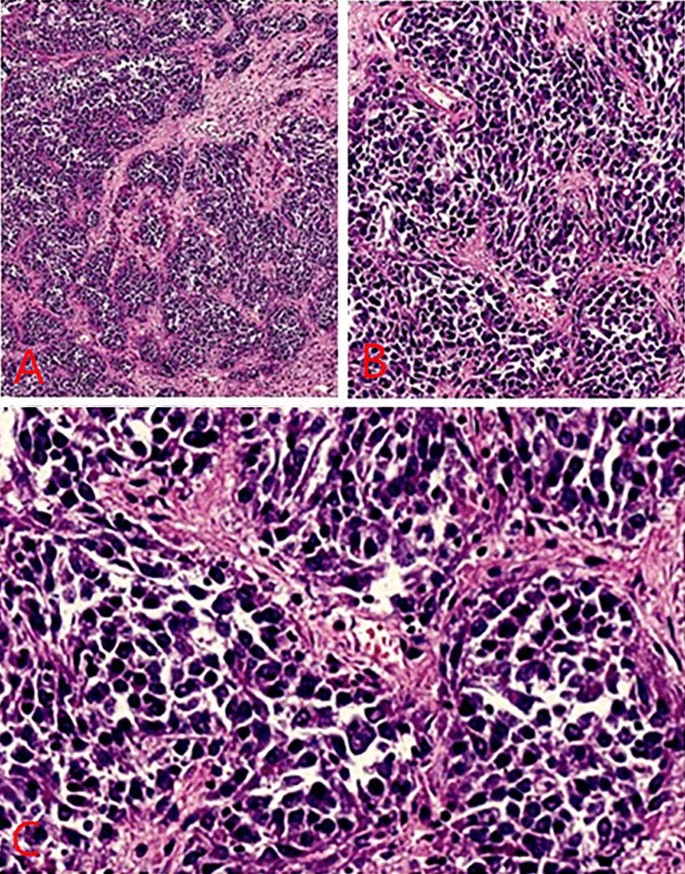
A Lymphoepithelioma-like carcinomas (staining, H&E; magnification, × 40). B High-power view of the same portion (staining, H&E; magnification, × 100). C Further high-power view revealed infiltrative growth of significant heterocyst nests in the liver tissue, which was morphologically consistent with malignant tumors, consider poorly differentiated carcinoma. (staining, H&E; magnification, × 200)
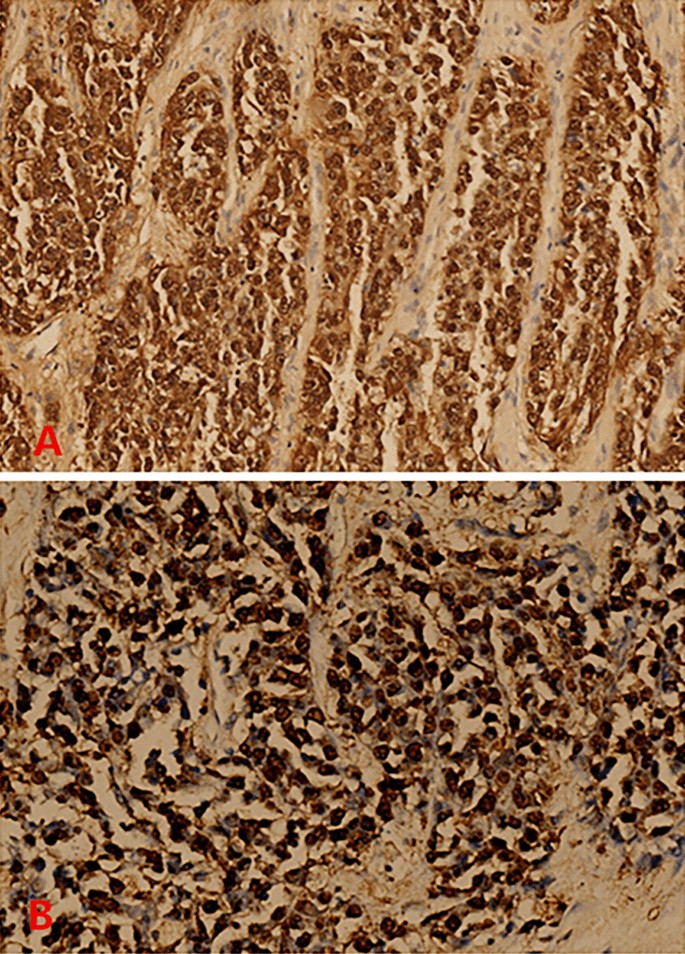
A Immunohistochemical results: CK7 foci (+), CK18 (weak + - +), CK19 (weak + - +), CK20 (−), CDX2 (weak + - +), AFP (−), Hepar1 (−), Arg-1 (−), GATA-3 (−), Vim (−), P40 a little (+), CD117 (−), CerbB2 (−), Ki-67 (+) 80–90%, EBV in situ hybridization: tumor cells EBER (+). Combining liver puncture with morphology, immunohistochemistry, and EBV in situ hybridization results, it was consistent with EB virus-associated poorly differentiated carcinoma (magnification, × 100). B Consider EBV infection-associated poorly differentiated cholangiocarcinoma (LELC morphology) magnification, × 200)
The Department of Infectious Diseases was invited for consultation, and the patient's pathology suggested EBV-related tumor. Upon inquiry of medical history, the patient often had fever from an early age, accompanied with tonsillitis and pus moss. The fever could be controlled after the use of antipyretics. The tonsils had been removed in 2015. In summary, EBV infection could be diagnosed. The patient was given intravenous drip of phosphopotassium sodium chloride injection (tolerable) 3g Q12h for antiviral symptomatic treatment. He was transferred to Shulan Hospital for liver transplantation. The patient underwent liver transplantation in Hangzhou Shulan Hospital on June 8, 2021, and the operation was successful. The pathology revealed EBV-related poorly differentiated cholangiocarcinoma. Regional lymph nodes: (groups 7, 8 and 9) 7/8 lymph node cancer metastases. After surgery, the patient orally took tacrolimus for anti-rejection, entecavir for antiviral therapy, gemcitabine 1.2 g combined with cis-platinum 30 mg for chemotherapy. With followed up for more than 5 months after liver transplantation, and the condition of the patient deteriorated. The patient is in critical condition currently, and the patient's family had given up treatment. The patient subsequently died. See Table 1 for patient condition and treatment process, and abbreviations

Comments
Post a Comment