What is Polio? - What is Polio
Is It COVID, Flu, Or Allergies? How To Protect Yourself And Loved Ones This Season
Flu season is here once again. And many questions have formed over the last couple of years about how you can stay safe from both the influenza (flu) and COVID-19 viruses, as well as how to tell if your symptoms may be caused by seasonal allergies or a different virus instead.
UChicago Medicine infectious diseases experts are here to help address your concerns and offer up some key advice on how to stay safe this season.
Below, Allison Bartlett, professor at University of Chicago Medicine and associate medical director of pediatric infection control, answers commonly asked questions.
Does COVID-19 or influenza pose a greater risk for people this season?Either virus can make you very sick or lead to death, which is why it's essential to get vaccinated and also to avoid close contact with others when sick. There are definitely populations that are more at risk for severe complications from each infection. Older adults and people with chronic underlying health conditions seem to be much more likely to get severely ill with COVID-19. And kids, especially infants under 1, and pregnant women are more likely to have severe infections with influenza.
Does having COVID-19 give you any antibodies against a respiratory virus like the flu?Unfortunately not. Having one virus does not protect you from the other.
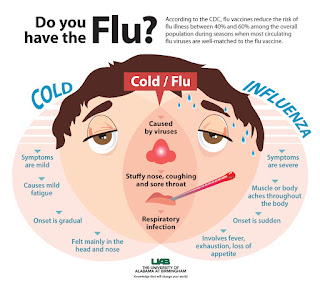
How can you tell if you have the flu, COVID-19, seasonal allergies or a different virus?The best way to tell what kind of respiratory virus you have is to get tested. Symptoms can be nearly impossible to tell apart. This is especially true between COVID-19 and the flu, with the notable exception that some people with COVID-19 lose their sense of taste and smell. Add in the fact that people can have one of these two viruses without symptoms, and it's basically impossible to tell one from the other on your own.
Testing determines the best treatment for your symptoms and how long you should stay home from work or school. The good news is that many health care providers who are doing coronavirus tests should be able to test you for the flu at the same time. There are many other viruses that can cause respiratory symptoms, so even if you test negative for COVID and flu, you should practice good respiratory hygiene: cover your cough, throw tissues away after use, wash your hands frequently.
What steps can you take to avoid getting COVID-19 and the flu?Many of the steps we take to protect ourselves from the coronavirus are the same things we need to do to keep us safe from influenza. The most important thing you can do to keep yourself and those around you safe from both viruses is to stay up-to-date on your COVID-19 and flu vaccinations.
You should get a flu shot even if you've already had the flu this season. The vaccine prevents against four different strains of the virus and we expect at least one more (Flu B) to be circulating later this season.
Practicing these good habits is also a great way to stay healthy:
The flu shot can help prevent people from becoming sick from influenza but won't provide specific protection against COVID-19. And the COVID-19 vaccine alone will not prevent you from getting the flu. It is strongly recommended that you receive both vaccines for maximum protection.
Can Tamiflu or the flu shot treat COVID-19?Tamiflu or a flu shot will not directly treat or lessen the symptoms of COVID-19. But you can get vaccinated against the flu and COVID-19, which can help prevent an infection and lessen severity. And if you get sick with influenza or have been exposed to it, you can take antiviral medication like oseltamivir (Tamiflu) to prevent getting sick.
COVID-19 treatment options are available and vary depending on the severity of your symptoms and health history. Antiviral treatments can help prevent the virus from spreading and avoid serious illness.
What should you do if you develop influenza or COVID-19 symptoms?If you have any symptoms, stay home, stay away from other people and try to isolate yourself to prevent the spread to others. Try to get tested within 48 hours of the start of your symptoms.
If it's influenza, your health care provider can prescribe medication to help your symptoms improve faster.
If it's COVID-19, your health care provider may recommend one of the treatment options referenced above.
Will the pneumonia vaccine protect me against the flu or COVID-19?The pneumonia vaccine helps protect against a variety of bacteria that can cause bacterial pneumonia. The pneumonia vaccine won't prevent flu or COVID-19, but it can help prevent complications that may come after.
Can I boost my immune systems to protect against flu or COVID-19?We wish there were a list of things we could do to help our immune systems prevent us from getting sick with the flu or the coronavirus. But there's no magic immune-boosting drug — only vaccination. Instead, focus on eating a healthy, varied diet and getting enough sleep. Also, make sure you've got any chronic medical conditions under control.
Can I do anything to decrease my chance of getting very sick if I've been exposed?Once an exposure to COVID-19 has happened, there's not a lot we can do to modify who gets sick from it. If you have been exposed to influenza, your physician may give you some medication like Relenza (zanamivir), Tamiflu (oseltamivir) and Rapivab (peramivir) within 48 hours of exposure. However, the best thing you can do is focus on avoiding exposure.
Are there new RSV vaccines available for adults?In 2023, there are finally ways to protect infants and loved ones from RSV during virus season. Nirsevimab is a newly-approved, one-time injection that provides immediate protection to infants 0 to 8 months old and reduces risk of RSV-related hospitalization significantly. All infants born at Comer Children's and Ingalls Memorial during RSV season will be offered this injection. Infants less that 8 months old at the start of RSV season can receive nirsevimab from their pediatrician and it can be given along with other routine immunizations.
UChicago Medicine is also offering two newly approved RSV vaccinations to eligible adults. A vaccine known as Abrysvo is available to pregnant individuals between their 32nd and 36th weeks. UChicago Medicine patients over 60 can also receive an RSV vaccine known as Arexvy. These adult vaccinations are available during physician office visits and both provide key protection for those at highest risk of severe RSV symptoms.
Have Your Cold Or Flu Symptoms Lingered This Winter? Doctors Explain Why.
It's a common complaint this winter: After coming down with a respiratory illness, some people feel like they can't shake a lingering cough or runny nose despite other symptoms going away. Or they start to recover then see symptoms return a week or two later.
Doctors say that course of events isn't unusual, though it might be more pronounced this year.
Covid, flu and respiratory syncytial virus (RSV) are all circulating widely. As of Dec. 16, flu hospitalizations had increased nearly 200% over the previous four weeks. And Covid hospitalizations increased around 40% over the four-week period ending Dec. 9, the latest data available.
NBC News spoke with seven doctors across seven states about why some people's symptoms can persist for weeks or months. They offered several possible explanations.
For one, the experts said, many people are more susceptible to respiratory illnesses this winter because they haven't had a recent infection or vaccination. Others may have gotten back-to-back infections that they confused with lingering symptoms.
It's also likely that, following the pandemic — when many common viruses weren't circulating widely — some people simply forgot how long symptoms can linger after a standard respiratory illness.
"It can take as long as two weeks or more to recover fully," said Dr. Linda Bell, South Carolina's state epidemiologist.
'Immunity debt' may be catching up to peopleBecause masking and isolation slowed the spread of many viruses during the pandemic, some people haven't been as exposed to flu or RSV over the last few years as they would have been. That can give rise to what doctors call "immunity debt" — decreased immunity that makes people more susceptible to infection.
"As more of us are encountering these viruses that we haven't seen in recent years, it might feel like some of them are a little bit more severe and we have some more severe symptoms than we had before," said Dr. Molly Fleece, a hospital epidemiologist at the University of Alabama at Birmingham Medicine.
A lack of vaccine-induced protection can also predispose people to more severe illness and make it harder to recover, doctors said.
The Centers for Disease Control and Prevention sent an alert to health care providers last week warning about low vaccination rates for Covid, flu and RSV.
RSV vaccines have been approved for older adults and pregnant people, but just 17% of those ages 60 and older had gotten an RSV shot as of Dec. 9. Meanwhile, the CDC reported a supply shortage for a newly approved RSV antibody injection for infants in October. However, additional doses became available last month, and 230,000 more are expected in January.
The flu vaccination rate so far this year is 42% for adults and 43% for children, compared with 47% and 57%, respectively, the previous season. Just 18% of adults and 8% of eligible children have received the newest Covid vaccine.
Last year, doctors said, masking and social distancing were also still more common.
"That may be why people are getting more sick now," said Dr. Caroline Goldzweig, chief medical officer of the Cedars-Sinai Medical Foundation in Los Angeles.
Two infections back to backSince this is only the second year with Covid, flu and RSV circulating widely at once, there may simply be more opportunities to get sick than in previous winters, doctors said.
"In the past several years, we've had primarily Covid or primarily RSV peaking, and now we have multiple respiratory viruses all rising at the same time," said Dr. Larissa Pisney, an infectious disease specialist at UCHealth in Aurora, Colorado.
That could raise the chance of back-to-back infections.
"It's entirely possible to be exposed to several different viruses over the course of the winter and have several different bouts of respiratory infection," said Dr. Daniel Ouellette, a pulmonary disease specialist at Henry Ford Health in Detroit.
It's also possible to get more than one virus at a time, though the CDC hasn't noticed that happening much, according to its director, Dr. Mandy Cohen.
"We see co-infections at about a similar level to this time last season," Cohen said.
However, several doctors said they're seeing an increase in bacterial infections — such as strep throat, whooping cough or pneumonia — that either follow a viral illness or occur at the same time.
"In some situations, having a viral respiratory illness increases your risk of having bacterial pneumonia, which we've classically seen for a long time with the flu, but then we also saw a little bit of that with Covid as well," said Dr. Shivanjali Shankaran, an infectious disease physician at Rush University Medical Group in Chicago.
It's normal for symptoms to linger or recurSymptoms that go away then reappear could be part of the same viral infection, said Dr. Donald Yealy, chief medical officer at the University of Pittsburgh Medical Center.
"You can have an initial infection, start to get better and then have some recrudescence — in other words, recurrence of the symptoms as you're recovering," he said. "People may mistake that for two separate infections."
It's also fairly common to feel sick for several weeks, doctors said. And Covid, flu and RSV can all result in a post-viral cough.
"That post-viral cough doesn't necessarily mean the person is still potentially able to spread the infection to others. It's just a residual effect of their prior infection," Fleece said.
But a small minority of people may not recover for months or years. Long Covid affects around 6% of U.S. Adults, according to a June survey by the Census Bureau. Similarly, it's possible to see lingering effects from flu or colds.
A study published last week showed that the flu can lead to a persistent cough or shortness of breath over the course of at least 18 months. And an analysis of U.K. Adults published in October found that common cold viruses can lead to coughing, stomach pain and diarrhea more than a month after an initial infection. Scientists are still trying to understand why.
What's Going Around: RSV, Strep, Flu, Stomach Bug
WellSpan Pediatric Medicine Physicians across the Midstate are seeing RSV, croup, bronchiolitis and flu.
The providers at UPMC Children's Community Pediatrics in York and Spring Grove are continuing to see RSV, strep throat and viral illness this week. They are also seeing a stomach bug.
The CVS MinuteClinic in York reports the flu and viral bronchitis this week.
Pediatricians at Penn State Health Children's Hospital continue to see a lot of RSV, some cases of COVID, some cases of the flu, strep throat, upper respiratory infections, bronchitis and stomach bugs.
Penn Medicine Lancaster General Health Physicians Roseville Pediatrics says RSV is still the most common virus they are seeing, although they saw a sharp increase in strep cases this week.
The flu and stomach bug have also been on the rise. They have seen a bit more croup in the last week and asthmatics have been having a rough time with the viral load in the community. They have seen an increase in asthma exacerbations as a result.
Dr. Joan Thode offered the following advice about strep and sore throats:
"Strep throat is caused by a bacteria called streptococcus, which is highly contagious and common especially in the winter months. While the typical clinical picture is a bad sore throat, other common symptoms of a strep infection include headache and belly pain, which often includes nausea and vomiting, but not diarrhea.
In older kids and adults, a strep infection can mimic symptoms of the flu, with fevers, body aches and fatigue. The only way to definitively differentiate the flu from strep is by a swab.
Strep does warrant treatment with antibiotics. We do not treat for strep without testing with a swab, however, because the antibiotic that would treat strep could cause bad side effects or bacterial resistance in the context of the other diagnoses. It takes an office visit to put your child's symptoms together with the physical exam and possibly an additional swab to make an accurate diagnosis.
Dangerous symptoms to watch for that warrant an immediate call to the doctor: difficulty swallowing to the point where your child is drooling because they cannot swallow their saliva; severe throat pain that is only on one side of the throat that causes their voice to become very whispery; sore throat accompanied by distressed breathing or the child's feeling like they can't inhale enough air."
For the latest news, weather, sports, and streaming video, head to ABC27.


Comments
Post a Comment